Every week, a multidisciplinary team of specialists from the McGill University Health Centre (MUHC) meets at the Cedars Cancer Centre to discuss their most complex melanoma cases and to decide on the best course of treatment and type of care they can provide to their patients. The team is made up of dermatologists, medical oncologists, surgical oncologists, plastic surgeons, head and neck surgeons, and dermatopathologists. Their unique, innovative approach is what makes the MUHC’s Melanoma Clinic the leader in melanoma treatment and care in Québec.
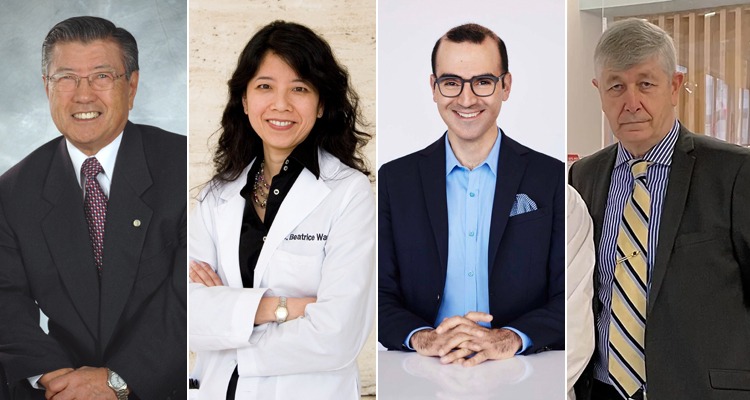
The Melanoma Clinic was founded at the Royal Victoria Hospital in 1970 by three young physicians who believed that immunotherapy was the future of melanoma treatment: surgical oncologist Henry Shibata, endocrinologist Martin Jerry and pathologist Martin Lewis. “Melanoma was seen as a mysterious and enigmatic type of cancer at the time. It was not well understood, and survival rates were very low,” recounts Dr. Shibata. “So, we decided to establish the first dedicated, multidisciplinary melanoma clinic in the country.” The rest is history.
The team initially started testing the efficacy of BCG, a vaccine for tuberculosis, in shrinking melanoma tumours. “Unfortunately, BCG turned out to be not very effective against melanoma, but extremely effective against bladder cancer,” says Dr. Shibata. Undeterred, he and his team moved on to other promising immunotherapy drugs, testing their efficacy in different doses and in conjunction with chemotherapy and surgery. Their work was truly groundbreaking, and, in just a matter of years, they had developed treatments that were safer and more effective – and that dramatically improved survival rates.
In 2005, Dr. Shibata handed-over the reins of the Melanoma Clinic to dermatologist and dermatological surgeon Dr. Beatrice Wang, who specializes in melanoma and other skin cancers. The clinic continues to lead the way in terms of immunotherapy-based treatments, and it has flourished under Dr. Wang’s leadership. “Today, our clinic is one of the largest in Canada. We receive referrals not only from Montréal but from across Québec and Eastern Canada, and we coordinate care with the outlying regions,” she says.
“Our team is multidisciplinary, made-up of a dynamic and diverse group of specialists who sub-specialize in melanoma.”
When asked to explain what makes the MUHC’s Melanoma Clinic so unique and successful, Dr. Wang explains: “Our team is multidisciplinary, made-up of a dynamic and diverse group of specialists who sub-specialize in melanoma. So, we’ve got the best minds pooling their expertise into developing the best possible treatment and care for our melanoma patients. The fact that we meet weekly, to gather the thoughts of all the specialists on each case, is of utmost importance.”
One of these talented specialists is Dr. Catalin Mihalcioiu, a medical oncologist whose team has implemented ground-breaking immunotherapy treatments that are helping to reduce the need for major surgery or prolonged treatments and are improving health outcomes for patients. In Quebec, the standard course of care for locally borderline advanced melanoma is to perform surgery on the tumour and to administer a year of post-surgery immunotherapy treatments. However, Dr. Mihalcioiu and his team are using a short course of dual immunotherapy treatments, that they administer before performing surgery, which has shown to be very effective at reducing tumours size. “If we are able to shrink the tumours beforehand, the surgery is less invasive, with less post-op complications,” explains Dr. Mihalcioiu. “For those patients achieving a complete response, one year of post-surgery adjuvant immunotherapy can be omitted, thereby avoiding potential autoimmune side effects and minimizing the cost.”
Another prominent member of the Melanoma Clinic team is Dr. Ari Meguerditchian, who performs pioneering, minimally invasive surgeries on patients with metastatic melanoma. “With such rapid advances in immunotherapy and targeted therapy, we are now able to optimize our treatment plans for each patient and each tumour, and we can perform more focused and less invasive surgery. Thanks to these innovative new treatments, there’s no more one-size-fits all approach, and patients are living better and living longer.”
“This is a very exciting field to be in,” says Dr. Wang. “The ways in which melanoma patients are being treated are changing exponentially, and the latest treatments are increasing survival rates, decreasing the morbidity of surgery, and, importantly, decreasing the overall amount of treatment that our patients require,” she concludes.
Jeff J. Shamie, President & CEO of the Cedars Cancer Foundation, couldn’t be more enthusiastic when asked about the Melanoma Clinic and the extraordinary results it’s achieving “We’ve literally got the most important and most innovative melanoma clinic in Québec right here at the MUHC, and Cedars is extremely proud to support its work.”
For more information, or to donate, please visit cedars.ca.
About Melanoma*
• Melanoma is one of the fastest growing cancers worldwide. In Canada, diagnosed cases of melanoma have more than tripled in the last 30 years and they continue to rise.
• Over 1,300 Canadians die from this disease each year.
• What makes this cancer so dangerous is its ability to metastasize (spread) easily to other parts of the body.
• The leading cause of melanoma is overexposure to ultraviolet (UV) radiation from the sun or artificial sources (like tanning beds and sunlamps).
• 85% of melanomas among Canadian men and women over the age of 30 can be attributed to UV radiation exposure.
*Source: Melanoma Canada